By accepting this disclaimer and continuing on this portal, I hereby confirm that I am a registered healthcare practitioner and I am authorized as per applicable laws to access the content shared on this portal. I acknowledge that the material and information shared on this portal is meant for limited access of a healthcare practitioners only and I will not share or distribute the confidential material and information shared with me on this portal with an unauthorized person. I confirm to not rely on the material and information shared herein and apply my independent medical judgement for assessing any patient.
Management
of Hemophilia

The main medication to treat hemophilia A is ‘concentrated FVIII’, also called clotting factor or simply ‘factor’. There are two types of clotting factors: Plasma-derived and Recombinant.
The other treatment options include cryoprecipitate, fresh frozen plasma, desmopressin. Since each person responds to treatment differently for a variety of reasons, an analysis of specific symptoms—such as bleeding rates and level of factor in the blood—can help doctors find the right treatment and regimen for a particular person with a bleeding disorder.
Episodic care
(On-demand therapy)
On-demand therapy is factor replacement therapy given to stop uncontrolled & spontaneous bleeding after bruising or injury.

Prophylactic care
(Prophylaxis treatment)

Prophylaxis is the regular use of clotting factor which prevents bleeding before it starts. Injections of clotting factor are given one, two or three times a week to maintain a constant level of these factors in the bloodstream so that severe bleeding episodes are avoided.
Conventional factor prophylaxis with standard half-life clotting factor is defined by intensity (these categories have not (as yet) been revised for use of EHL* clotting factors or non-factor therapies).
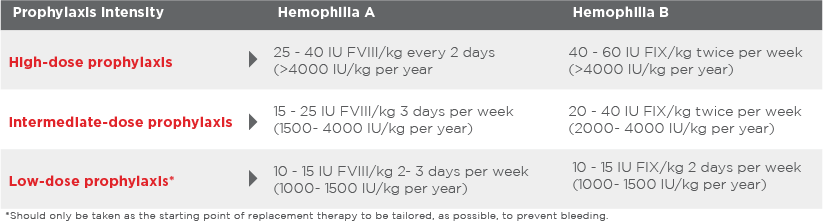
EHL - Extended Half Life
World Federation of Hemophilia recommends
Prophylaxis because…
Prophylaxis is a preventive measure in hemophilia where regular infusion of blood clotting factor
concentrates helps avoid bleeding and its long term consequences.
Inhibitor therapy
Inhibitors complicate hemophilia treatment
About 20-30 percent of people with Hemophilia A develop an antibody (called an inhibitor) to the factor therapy. This antibody stops the clotting factors in the therapy from being able to clot the blood and stop bleeding. Treatment of bleeding episodes becomes extremely difficult, and the cost of care for a person with an inhibitor escalates because more clotting factor or a different type of clotting factor is needed.
People with inhibitors often experience more joint disease and other problems from bleeding that result in a reduced quality of life.
Special blood products, called bypassing agents, are used to treat bleeding episodes for people with high titer inhibitors. Instead of replacing the missing factor, they go around (or bypass) the factors that are blocked by the inhibitor to help the body form a normal clot.
Alternately Immune Tolerance Induction (ITI) Therapy can be prescribed. With ITI therapy, people receive large amounts of factor every day for many weeks or months.
Approximately 1 in 5 people with hemophilia¹ and about 3 in 100 people with hemophilia² will develop an antibody-called an inhibitor-to the treatment product (medicine) used to treat or prevent their bleeding episodes.
The healthcare costs associated with inhibitors can be staggering because of the amount and type of treatment product required to stop bleeding. Also, people with hemophilia who develop an inhibitor are twice as likely to be hospitalized for a bleeding complication, and they are at increased risk of death.3,4,5